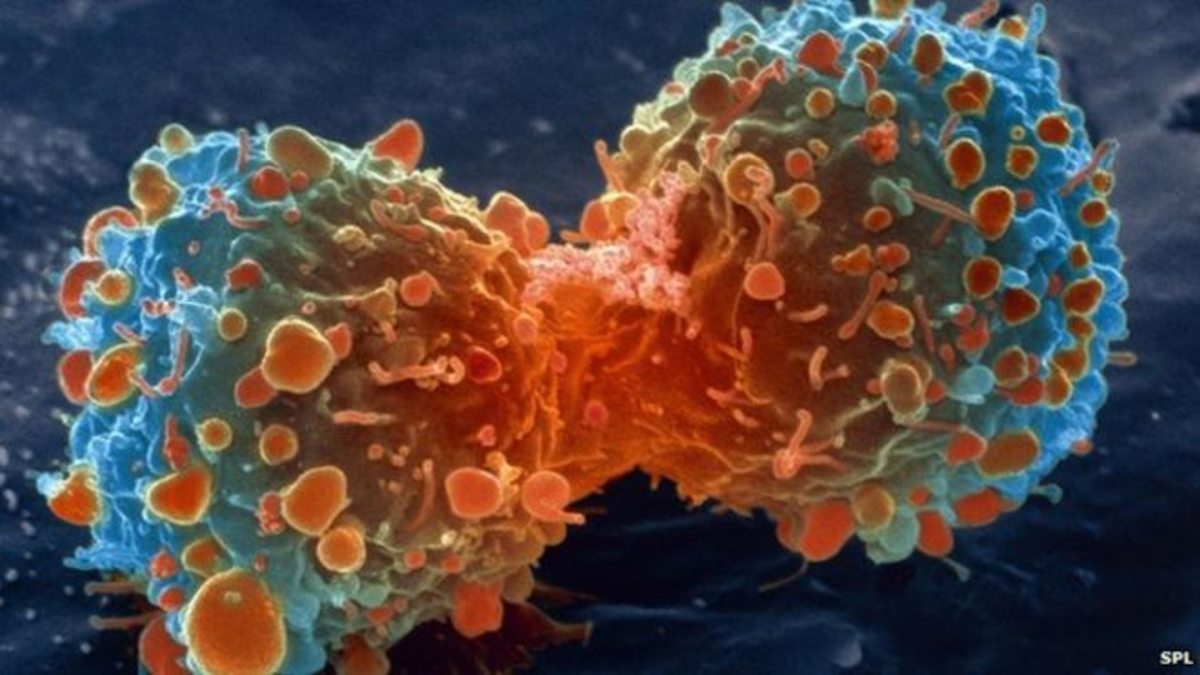
Cancer cell during cell division. Credit: National Institutes of Health
A collaboration between Saïd M. Sebti, Ph.D., chair of Moffitt Cancer Center’s Drug Discovery Department, and Michele Pagano, M.D., chair of the Department of Biochemistry and Molecular Pharmacology at New York University’s Langone Medical Center, led to the publication of an important study in the latest issue of Nature. The investigation found that the drug, geranylgeranyltransferase inhibitor GGTI-2418 suppresses a new defective PTEN cancer pathway discovered by Pagano’s group.
Fully functional PTEN is well known to suppress tumor growth by antagonizing the PI3K/Akt tumor survival pathway. Pagano’s group discovered a novel mechanism by which PTEN protects cells from cancer by preventing the geranylgeranylated protein FBXL2 from binding and degrading IP3R3. IP3R3 is an important anti-cancer “sensor” recognizing hyper-proliferating cells that use abnormally high levels of energy, and targeting them to self-destruct as an anti-cancer safety mechanism. The PTEN gene binds to IP3R3, protecting its cancer-sensing function. However PTEN is defective in many cancers, and as such, FBXL2 is left unchecked; too much IP3R3 is degraded and fast-multiplying cells are less able to self-destruct.
“FXBL2 may be partially responsible for cancer growth in the many patients with genetic changes that happen to disable PTEN,” said Pagano. The drug GGTI-2418 blocks this cancer-causing activity of FBXL2 by inhibiting its geranylgeranylation which is required for FBXL2 to bind and degrade IP3R3. GGTI-2418 was co-discovered and developed by Sebti and NYU President Andrew Hamilton, Ph.D., while he was at Yale University. .
Another fascinating consequence of this discovery is that cancers with defective PTEN activate two tumor survival circuits to evade cell death, the PI3K/Akt and the FBXL2 pathways. “These findings have important translational implications as patients whose tumors harbor defective PTEN may benefit greatly from a combination of inhibitors of FBXL2 geranylgeranylation, such as GGTI-2418, and inhibitors of Akt, such as TCN-P,” said Sebti. Both GGTI-2418 and TCN-P were co-discovered by Sebti and are now developed by the clinical-stage oncology company Prescient Therapeutics Ltd.
The researchers also found that using GGTI-2418 to block FBXL2 from degrading IP3R3 made the tumors in mice more vulnerable to photodynamic therapy (PDT).”This experimental drug, by itself and with a form of light therapy, countered FBXL2 to let abnormal cells self-destruct,” said Pagano “We will be looking to collaborate with Dr. Sebti on clinical studies combining GGTI-2418 with PDT or TCN-P in patients with low PTEN.”
Explore further:
Scientists discover metabolic pathway that drives tumor growth in aggressive cancers
More information:
Shafi Kuchay et al. PTEN counteracts FBXL2 to promote IP3R3- and Ca2+-mediated apoptosis limiting tumour growth, Nature (2017). DOI: 10.1038/nature22965
__
This article and images was originally posted on [Medical Xpress] June 14, 2017 at 03:05PM
Provided by: H. Lee Moffitt Cancer Center & Research Institute